用户:Kaguya-Taketori/巨核细胞
| 巨核细胞 | |
|---|---|
 巨核细胞 | |
 骨髓中的巨核细胞 | |
| 标识字符 | |
| 拉丁文 | megakaryocytus |
| 《解剖学术语》 [在维基数据上编辑] | |
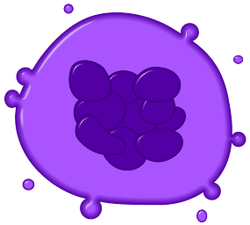
巨核细胞(mega- + karyo- + -cyte)是一种大型的骨髓细胞。它有一个负责制造血小板(一种为正常的凝血过程所必须的物质)的分叶状细胞核。一般情况下,每10000个骨髓细胞中会有一个巨核细胞,但是当肌体患上某些疾病时,巨核细胞的数目可以增加近10倍[1]。
结构
[编辑]一般说来,巨核细胞的大小是红细胞的10-15倍,其平均直径可达50-100微米(μm)。巨核细胞在发育过程中,细胞大小会不断增加,DNA会在不进行有丝分裂的前提下不断复制。因为DNA的不断复制,巨核细胞的细胞核会变得很大,而且呈现分叶状。如果用光镜观察的话,观察者很容易误认为巨核细胞有多个细胞核。有时,巨核细胞的细胞核中染色体可达64组(人的一个染色体组有23条染色体,正常人的体细胞中含有2个染色体组)。
巨核细胞的细胞质基质中含有α颗粒以及。血小板可以认为是从巨核细胞上单独分离出来的小块细胞质。
巨核细胞的发育
[编辑]
巨核细胞可由造血干细胞(一类具有全能性的细胞,可根据接收到的信号的不同分化为不同的血细胞)在骨髓内分化而来。促血小板生成素(Thrombopoietin,简称TPO)可以诱导造血干细胞分化为巨核细胞,但也有其它可达到同样的效果的途径[2],比如说GM-CSF、IL-3、IL-6、IL-11、趋化因子SDF-1、FGF-4[3]、促红细胞生成素都可以诱导造血干细胞分化为巨核细胞[4]。巨核细胞的发育过程如下:
造血干细胞分化为巨核细胞后会丧失分裂能力。但是,巨核细胞却能够在不分裂的情况下持续进行生长和DNA复制[4]。人的巨核细胞染色体组数可达64组,而老鼠的巨核细胞染色体组数则可达256组(人和老鼠都是二倍体,即正常情况下体细胞内有2个染色体组)。如果诱导非造血细胞表达第六类β微管蛋白(β6)的话,相关细胞也会表现出不少为巨核细胞分化所特有的形态特征。这一事实可以帮助人们更好地理解造血干细胞分化形成巨核细胞的过程[5]。
释放血小板
[编辑]巨核细胞在成熟过程中,会在不分裂的情况下对核DNA进行复制。巨核细胞在完全成熟后,就会开始制造血小板[6]。促血小板生成素能够诱导巨核细胞产生血小板。尚未被释放的血小板被裹在巨核细胞细胞质基质内的膜中。目前,学者总共提出了两种血小板可能的释放机制。其中一种假说认为,巨核细胞通过让这些膜解体来释放膜内的血小板[7]。该假说还指出,巨核细胞也能把一种血小板细带释放到血管中。这种细带带有伪足,并能持续地把血小板送入血液循环中。另一种假说则认为,上述的血小板形成过程一次能够产生2000-5000个新的血小板。
新产生的血小板有2/3会进入血循环中,另外1/3则会被脾脏暂时储存起来。
在产生了一定数量的血小板后,巨核细胞就只剩下细胞核了。这样的巨核细胞会穿过骨髓的血液屏障,进入肺中,然后被肺泡巨噬细胞消化掉。
Effects of cytokines
[编辑]Cytokines are signals used in the immune system for intercellular communication. There are many cytokines that affect megakaryocytes. Certain cytokines such as IL-3, IL-6, IL-11, LIF, erythropoietin, and thrombopoietin all stimulate the maturation of megakaryocytic progenitor cells.[8] Other signals such as PF4, CXCL5, CXCL7, and CCL5 inhibit platelet formation.[9]
Thrombopoietin
[编辑]Thrombopoietin (TPO) is a 353-amino acid protein located on chromosome 3p27. TPO is primarily synthesized in the liver[10] but can be made by kidneys, testes, brain, and even bone marrow stromal cells. It has high homology with erythropoietin. It is essential for the formation of an adequate quantity of platelets. Mice lacking TPO or the TPO receptor (Mpl) have a 90% reduction in circulating platelet number, although the platelets are normal in morphology and function.[11]
Disorders involving megakaryocytes
[编辑]Megakaryocytes are directly responsible for producing platelets, which are needed for the formation of a thrombus, or blood clot. There are several diseases that are directly attributable to abnormal megakaryocyte function or abnormal platelet function.[12]
Essential Thrombocythemia
[编辑]Essential thrombocytosis (ET-Also known as Essential thrombocythemia) is a disorder characterized by extremely high numbers of circulating platelets. The disease occurs in 1-2 per 100,000 people. The current WHO requirements for diagnosis include > 600,000 platelets/μL of blood (normal 150,000-400,000) and a bone marrow biopsy. Some of the consequences of having such high numbers of platelets include thrombosis or clots throughout the body. Thrombi form more frequently in arteries than veins. It seems ironic that having platelet counts above 1,000,000 platelets/μL can lead to hemorrhagic events.[13] Recent evidence suggests that the majority of ET cases are due to a mutation in the JAK2 protein, a member of the JAK-STAT pathway.[14] Evidence suggests that this mutation renders the megakaryocyte hypersensitive to thrombopoietin and causes clonal proliferation of megakaryocytes. There is a significant risk of transformation to leukemia with this disorder. The primary treatment consists of anagrelide or hydroxyurea to lower platelet levels.
Congenital amegakaryocytic thrombocytopenia (CAMT)
[编辑]Congenital amegakaryocytic thrombocytopenia (CAMT) is a rare inherited disorder. The primary manifestations are thrombocytopenia and megakaryocytopenia, i.e. low numbers of platelets and megakaryocytes. There is an absence of megakaryocytes in the bone marrow with no associated physical abnormalities.[15] The cause for this disorder appears to be a mutation in the gene for the TPO receptor, c-mpl, despite high levels of serum TPO.[16][17] In addition, there may be abnormalities with the central nervous system including the cerebrum and cerebellum that could cause symptoms.[16] The primary treatment for CAMT is bone marrow transplantation.
Bone marrow/stem cell transplant is the only remedy for this genetic disease. Frequent platelet transfusions are required to keep the patient from bleeding to death until transplant has been completed, although this is not always the case.
One of the few non-medical research related sources on the web with some information on CAMT is:
There appears to be no generic resource for CAMT patients on the web and this is potentially due to the rarity of the disease.
External links
[编辑]- Megakaryocytes: Mature Many microscopic images of mature megakaryocytes including in disease settings.
- Cell size comparison
- CAMT Specific Infant Bone Marrow Transplant Journal
- ^ Branehog I, Ridell B, Swolin B, Weinfeld A. Megakaryocyte quantifications in relation to thrombokinetics in primary thrombocythaemia and allied diseases. Scand. J. Haematol. 1975, 15 (5): 321–332. PMID 1060175. doi:10.1111/j.1600-0609.1975.tb01087.x.
- ^ Bunting S, Widmer R, Lipari T, Rangell L, Steinmetz H, Carver-Moore K, Moore MW, Keller GA, de Sauvage FJ. Normal platelets and megakaryocytes are produced in vivo in the absence of thrombopoietin. Blood. November 1997, 90 (9): 3423–3429. PMID 9345025.
- ^ Avecilla ST, Hattori K, Heissig B, Tejada R, Liao F, Shido K, Jin DK, Dias S, Zhang F, Hartman TE, Hackett NR, Crystal RG, Witte L, Hicklin DJ, Bohlen P, Eaton D, Lyden D, de Sauvage F, Rafii S. Chemokine-mediated interaction of hematopoietic progenitors with the bone marrow vascular niche is required for thrombopoiesis. Nat Med. January 2004, 10 (1): 64–71. PMID 14702636. doi:10.1038/nm973.
- ^ 4.0 4.1 Deutsch VR, Torner A. Megakaryocyte development and platelet production. Brit. J. Haem. September 2006, 134 (5): 453–466. PMID 16856888. doi:10.1111/j.1365-2141.2006.06215.x.
- ^ Yang, H; Ganguly, A; Cabral, F. Megakaryocyte Lineage Specific Class VI β-Tubulin Suppresses Microtubule Dynamics, Fragments Microtubules, and Blocks Cell Division.. Cytoskeleton. 2012, 68 (3): 175–187. PMID 21309084. doi:10.1002/cm.20503.
- ^ January 2013 Megakaryocyte and Platelet Production 请检查
|url=值 (帮助). - ^ Choi ES, Nichol JL, Hokom MM; et al. Platelets generated in vitro from proplatelet-displaying human megakaryocytes are functional. Blood. 1995, 85 (2): 402–13. PMID 7529062.
- ^ Gordon MS, Hoffman R. Growth factors affecting human thrombocytopoiesis: potential agents for the treatment of thrombocytopenia. Blood. 1992, 80 (2): 302–307. PMID 1627792.
- ^ Pang L, Weiss MJ, Poncz M. Megakaryocyte biology and related disorders. J. Clin. Invest. 2005, 115 (12): 3332–3338. PMC 1297258
 . PMID 16322777. doi:10.1172/JCI26720.
. PMID 16322777. doi:10.1172/JCI26720.
- ^ Jelkmann W. The role of the liver in the production of thrombopoietin compared with erythropoietin. Eur. J. Gastroenterol. Hepatol. 2001, 13 (7): 791–801. PMID 11474308. doi:10.1097/00042737-200107000-00006.
- ^ Murone M, Carpenter DA, de Sauvage FJ. Hematopoietic deficiencies in c-mpl and TPO knockout mice. Stem Cells. 1998, 16 (1): 1–6. PMID 9474742. doi:10.1002/stem.160001.
- ^ Nurden AT. Qualitative disorders of platelets and megakaryocytes. J. Thromb. And Haem. 2005, 3 (8): 1773–1782. PMID 16102044. doi:10.1111/j.1538-7836.2005.01428.x.
- ^ Michiels JJ, Berneman ZN, Schroyens W, Van Vliet HH. Pathophysiology and treatment of platelet-mediated microvascular disturbances, major thrombosis and bleeding complications in essential thrombocythaemia and polycythaemia vera. Platelets. 2004, 15 (2): 67–84. PMID 15154599. doi:10.1080/09537100310001646969.
- ^ Kralovics R, Passamonti F, Buser AS, Teo SS; et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005-04-28, 352 (17): 1779–90. PMID 15858187. doi:10.1056/NEJMoa051113.
- ^ Freedman MH, Estrov Z. Congenital amegakaryocytic thrombocytopenia: an intrinsic hematopoietic stem cell defect. Am. J. Pediatr. Hematol. Oncol. 1990, 12 (2): 225–230. PMID 2378417. doi:10.1097/00043426-199022000-00020.
- ^ 16.0 16.1 Ihara K, Ishii E, Eguchi M, Takada H, Suminoe A, Good RA, Hara T. Identification of mutations in the c-mpl gene in congenital amegakaryocytic thrombocytopenia. Proc. Natl. Acad. Sci. 1999, 96 (6): 3133–6. PMC 15907
 . PMID 10077649. doi:10.1073/pnas.96.6.3132.
. PMID 10077649. doi:10.1073/pnas.96.6.3132.
- ^ Ballmaier M, Germeshausen M, Schulze H, Cherkaoui K, Lang S, Gaudig A, Krukemeier S, Eilers M, Strauss G, Welte K. C-mpl mutations are the cause of congenital amegakaryocytic thrombocytopenia. Blood. 2001, 97 (1): 139–46. PMID 11133753. doi:10.1182/blood.V97.1.139.
