二甲雙胍
此條目可參照英語維基百科相應條目來擴充,此條目在對應語言版為高品質條目。 (2023年12月24日) |
 | |
 | |
| 臨床資料 | |
|---|---|
| 讀音 | /mɛtˈfɔːrmɪn/, met-FAWR-min |
| 商品名 | Glucophage, other |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696005 |
| 核准狀況 | |
| 懷孕分級 |
|
| 給藥途徑 | 口服 |
| ATC碼 | |
| 法律規範狀態 | |
| 法律規範 |
|
| 藥物動力學數據 | |
| 生物利用度 | 50–60%[1][2] |
| 血漿蛋白結合率 | 很小[1] |
| 藥物代謝 | 不經過肝臟[1] |
| 生物半衰期 | 4-8.7小時[1] |
| 排泄途徑 | 尿液(90%)[1] |
| 識別資訊 | |
| |
| CAS號 | 657-24-9 |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.010.472 |
| 化學資訊 | |
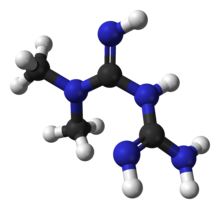
| 化學式 | C4H11N5 |
| 摩爾質量 | 129.17 g·mol−1 |
| 3D模型(JSmol) | |
| |
| |
二甲雙
二甲雙胍在人體通常沒有顯著副作用[8]。常見副作用包含腹瀉、惡心,以及腹痛[3],造成低血糖的機會不大[3]。但值得關注的是,不當用藥可能會導致乳酸中毒,嚴重者甚至會死亡[9]。肝病、腎功能衰竭者不宜服用本品[3],妊娠期間用藥目前沒有已知影響,但妊娠糖尿病一般建議以胰島素進行治療[3][10]。本品屬於雙胍類藥物[3],藉由降低肝臟糖質新生及提升胰島素敏感度來達到治療的效果[3]。
二甲雙胍最早於1922年發現[11],但直到1950年代,法國內科醫師讓·斯特恩(Jean Sterne)開啟了二甲雙胍人類應用的臨床研究[11]。1957年,本品開始在法國用於藥用,並於1995年開始於美國使用[3][12]。本品列名於世界衛生組織基本藥物標準清單之中,為基礎公衛體系必備藥物之一[13]。目前相信口服給藥是最有效的給藥途徑[11],本品屬於通用名藥物[3]。2014年本品於發達國家的批發價為0.21至5.55美元之間[14]。在美國,一個月療程的藥物花費約於 5 至 25 美元之間[3]。


藥理
[編輯]二甲雙胍的分子藥理機制目前尚不完全清楚。已知其至少作用於肝臟,減少糖異生(即葡萄糖的生產)與減輕胰島素抵抗[15]。有研究表明二甲雙胍可激活單磷酸腺苷活化的蛋白激酶(AMP-activated protein kinase,AMPK),是二甲雙胍抑制肝臟糖異生、在胰島素信號傳導通路中提高胰島素的敏感性不可缺少的機制之一[16]。AMPK作為蛋白激酶不僅在胰島素信號傳導通路中,在全身能量平衡以及葡萄糖和脂肪的代謝中也起着重要作用[17]。動物實驗和臨床研究均表明二甲雙胍可誘導糖尿病的糞便微生物菌群構成發生重大變化,不僅可能有助於胰高血糖素樣肽-1(GLP-1)的分泌及作用,還證實可改善胰島素的敏感性,也是其抗2型糖尿病作用的重要機制之一[18][19]。
優勢
[編輯]- 不會增加體重
- 與其他藥品相比不易造成低血糖
- 減少三酸甘油酯
- 對低密度脂蛋白有很好的效果
- 對血壓無影響
- 價格低廉
缺點
[編輯]研究
[編輯]有被研究用於非酒精性脂肪肝[20][21][22]和早發育[23][24][25]。
抗衰老
[編輯]一些資料顯示,服用二甲雙胍的糖尿病患者,其存活率甚至超過其他條件類似但未患糖尿病的人群[26],而對二甲雙胍在人類身上是否有抗衰老效果的臨床實驗預計於2016年冬在美國開始進行。流行病學研究表明,可預防心臟病、癌症和阿茲海默症等, 令致死疾病減少身體較健康,食十年以上整體增加一成多壽命。 [27]
對動物模型有顯著的延壽作用。[28]目前尚無質量足夠的人類臨床研究證明其延長壽命。對於不患糖尿病的人未觀測到降低癌症、心血管疾病發病率的情況。[29]對於糖尿病患者則確實有抗癌、抗心血管疾病的現象,甚至和血糖控制情況是獨立的。[30][31]
不排除其可以延長「無病壽命」的可能性。[32]
註解
[編輯]參考文獻
[編輯]- ^ 1.0 1.1 1.2 1.3 1.4 Dunn CJ, Peters DH. Metformin. A review of its pharmacological properties and therapeutic use in non-insulin-dependent diabetes mellitus. Drugs. May 1995, 49 (5): 721–49. PMID 7601013. doi:10.2165/00003495-199549050-00007.
- ^ Hundal RS, Inzucchi SE. Metformin: new understandings, new uses. Drugs. 2003, 63 (18): 1879–94. PMID 12930161. doi:10.2165/00003495-200363180-00001.
- ^ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 Metformin Hydrochloride. The American Society of Health-System Pharmacists. [Jan 2016]. (原始內容存檔於2016-12-24).
- ^ Maruthur, NM; Tseng, E; Hutfless, S; Wilson, LM; Suarez-Cuervo, C; Berger, Z; Chu, Y; Iyoha, E; Segal, JB; Bolen, S. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis.. Annals of Internal Medicine. 19 April 2016. PMID 27088241. doi:10.7326/M15-2650.
- ^ Clinical Obesity. 2nd. Oxford: John Wiley & Sons. 2008: 262 [2016-09-07]. ISBN 9781405143660. (原始內容存檔於2020-09-14).
- ^ Malek, M; Aghili, R; Emami, Z; Khamseh, ME. Risk of Cancer in Diabetes: The Effect of Metformin. (PDF). ISRN Endocrinology. 2013, 2013: 636927 [2016-09-07]. PMC 3800579
 . PMID 24224094. doi:10.1155/2013/636927. (原始內容存檔 (PDF)於2017-09-08).
. PMID 24224094. doi:10.1155/2013/636927. (原始內容存檔 (PDF)於2017-09-08).
- ^ 7.0 7.1 Type 2 diabetes and metformin. First choice for monotherapy: weak evidence of efficacy but well-known and acceptable adverse effects.. Prescrire international. November 2014, 23 (154): 269–72. PMID 25954799.
- ^ Triggle, CR; Ding, H. Metformin is not just an antihyperglycaemic drug but also has protective effects on the vascular endothelium.. Acta physiologica (Oxford, England). 17 December 2015. PMID 26680745. doi:10.1111/apha.12644.
- ^ Lipska KJ, Bailey CJ, Inzucchi SE. Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care. June 2011, 34 (6): 1431–7. PMC 3114336
 . PMID 21617112. doi:10.2337/dc10-2361.
. PMID 21617112. doi:10.2337/dc10-2361.
- ^ Lautatzis, ME; Goulis, DG; Vrontakis, M. Efficacy and safety of metformin during pregnancy in women with gestational diabetes mellitus or polycystic ovary syndrome: a systematic review.. Metabolism: clinical and experimental. November 2013, 62 (11): 1522–34. PMID 23886298. doi:10.1016/j.metabol.2013.06.006.
- ^ 11.0 11.1 11.2 Fischer, Janos. Analogue-based Drug Discovery II. John Wiley & Sons. 2010: 47–49 [2016-09-07]. ISBN 9783527632121. (原始內容存檔於2020-12-09).
- ^ McKee, Mitchell Bebel Stargrove, Jonathan Treasure, Dwight L. Herb, nutrient, and drug interactions : clinical implications and therapeutic strategies. St. Louis, Mo.: Mosby/Elsevier. 2008: 217 [2016-09-07]. ISBN 9780323029643. (原始內容存檔於2020-09-14).
- ^ WHO Model List of EssentialMedicines (PDF). World Health Organization. October 2013 [22 April 2014]. (原始內容存檔 (PDF)於2016-04-11).
- ^ Metformin. [11 January 2016].[永久失效連結]
- ^ How does this medication work?. OnlineClinic. [2015-01-30]. (原始內容存檔於2016-07-22).
- ^ Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, et al. Role of AMP-activated protein kinase in mechanism of metformin action. The Journal of Clinical Investigation. October 2001, 108 (8): 1167–74. PMC 209533
 . PMID 11602624. doi:10.1172/JCI13505 (英語).
. PMID 11602624. doi:10.1172/JCI13505 (英語).
- ^ Towler MC, Hardie DG. AMP-activated protein kinase in metabolic control and insulin signaling. Circulation Research. February 2007, 100 (3): 328–41. PMID 17307971. doi:10.1161/01.RES.0000256090.42690.05 (英語).
- ^ Burcelin R. The antidiabetic gutsy role of metformin uncovered?. Gut. May 2014, 63 (5): 706–7. PMID 23840042. doi:10.1136/gutjnl-2013-305370 (英語).
- ^ Wu, Hao; Esteve, Eduardo; Tremaroli, Valentina; Khan, Muhammad Tanweer; Caesar, Robert; Mannerås-Holm, Louise; 等. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nature Medicine. 2017-07, 23 (7): 850–858 [2021-04-11]. ISSN 1546-170X. doi:10.1038/nm.4345. (原始內容存檔於2017-12-11) (英語).
- ^ Jalali M, Rahimlou M, Mahmoodi M, Moosavian SP, Symonds ME, Jalali R, Zare M, Imanieh MH, Stasi C. The effects of metformin administration on liver enzymes and body composition in non-diabetic patients with non-alcoholic fatty liver disease and/or non-alcoholic steatohepatitis: An up-to date systematic review and meta-analysis of randomized controlled trials. Pharmacological Research. September 2020, 159: 104799. PMID 32278041. S2CID 215741792. doi:10.1016/j.phrs.2020.104799.
- ^ Blazina I, Selph S. Diabetes drugs for nonalcoholic fatty liver disease: a systematic review. Systematic Reviews //www.ncbi.nlm.nih.gov/pmc/articles/PMC6884753
|PMC=缺少標題 (幫助). November 2019, 8 (1): 295. PMC 6884753 . PMID 31783920. doi:10.1186/s13643-019-1200-8
. PMID 31783920. doi:10.1186/s13643-019-1200-8  .
.
- ^ Leoni S, Tovoli F, Napoli L, Serio I, Ferri S, Bolondi L. Current guidelines for the management of non-alcoholic fatty liver disease: A systematic review with comparative analysis. World Journal of Gastroenterology //www.ncbi.nlm.nih.gov/pmc/articles/PMC6092580
|PMC=缺少標題 (幫助). August 2018, 24 (30): 3361–3373. PMC 6092580 . PMID 30122876. doi:10.3748/wjg.v24.i30.3361
. PMID 30122876. doi:10.3748/wjg.v24.i30.3361  .
.
- ^ Ibáñez L, Ong K, Valls C, Marcos MV, Dunger DB, de Zegher F. Metformin treatment to prevent early puberty in girls with precocious pubarche. The Journal of Clinical Endocrinology and Metabolism. August 2006, 91 (8): 2888–91. PMID 16684823. doi:10.1210/jc.2006-0336
 .
.
- ^ Ibáñez L, López-Bermejo A, Díaz M, Marcos MV, de Zegher F. Early metformin therapy (age 8-12 years) in girls with precocious pubarche to reduce hirsutism, androgen excess, and oligomenorrhea in adolescence. The Journal of Clinical Endocrinology and Metabolism. August 2011, 96 (8): E1262–7. PMID 21632811. doi:10.1210/jc.2011-0555
 .
.
- ^ Ibáñez L, Díaz R, López-Bermejo A, Marcos MV. Clinical spectrum of premature pubarche: links to metabolic syndrome and ovarian hyperandrogenism. Reviews in Endocrine & Metabolic Disorders. March 2009, 10 (1): 63–76. PMID 18726694. S2CID 9129907. doi:10.1007/s11154-008-9096-y.
- ^ Bannister, C. A.; Holden, S. E.; Jenkins-Jones, S.; Morgan, C. Ll; Halcox, J. P.; Schernthaner, G.; Mukherjee, J.; Currie, C. J. Can people with type 2 diabetes live longer than those without? A comparison of mortality in people initiated with metformin or sulphonylurea monotherapy and matched, non-diabetic controls. Diabetes, Obesity & Metabolism. 2014-11, 16 (11): 1165–1173 [2021-08-12]. ISSN 1463-1326. PMID 25041462. doi:10.1111/dom.12354. (原始內容存檔於2022-04-05).
- ^ 世界首例抗衰老药将临床试验 或让人活到120岁. 中新網. 2015-12-02 [2015-12-02]. (原始內容存檔於2020-09-16).
- ^ Barzilai N, Crandall JP, Kritchevsky SB, Espeland MA. Metformin as a Tool to Target Aging. Cell Metabolism. June 2016, 23 (6): 1060–1065. PMC 5943638
 . PMID 27304507. doi:10.1016/j.cmet.2016.05.011.
. PMID 27304507. doi:10.1016/j.cmet.2016.05.011.
- ^ Lee CG, Heckman-Stoddard B, Dabelea D, Gadde KM, Ehrmann D, Ford L, Prorok P, Boyko EJ, Pi-Sunyer X, Wallia A, Knowler WC, Crandall JP, Temprosa M. Effect of Metformin and Lifestyle Interventions on Mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care //www.ncbi.nlm.nih.gov/pmc/articles/PMC8669534
|PMC=缺少標題 (幫助). December 2021, 44 (12): 2775–2782. PMC 8669534 . PMID 34697033. doi:10.2337/dc21-1046
. PMID 34697033. doi:10.2337/dc21-1046  .
.
- ^ Zhang J, Wen L, Zhou Q, He K, Teng L. Preventative and Therapeutic Effects of Metformin in Gastric Cancer: A New Contribution of an Old Friend. Cancer Management and Research //www.ncbi.nlm.nih.gov/pmc/articles/PMC7505710
|PMC=缺少標題 (幫助). 16 September 2020, 12: 8545–8554. PMC 7505710 . PMID 32982447. doi:10.2147/CMAR.S264032
. PMID 32982447. doi:10.2147/CMAR.S264032  (English).
(English).
- ^ Campbell JM, Bellman SM, Stephenson MD, Lisy K. Metformin reduces all-cause mortality and diseases of ageing independent of its effect on diabetes control: A systematic review and meta-analysis. Ageing Research Reviews. November 2017, 40: 31–44. PMID 28802803. S2CID 20334490. doi:10.1016/j.arr.2017.08.003.
- ^ Mohammed I, Hollenberg MD, Ding H, Triggle CR. A Critical Review of the Evidence That Metformin Is a Putative Anti-Aging Drug That Enhances Healthspan and Extends Lifespan. Frontiers in Endocrinology //www.ncbi.nlm.nih.gov/pmc/articles/PMC8374068
|PMC=缺少標題 (幫助). 2021, 12: 718942. PMC 8374068 . PMID 34421827. doi:10.3389/fendo.2021.718942
. PMID 34421827. doi:10.3389/fendo.2021.718942  .
.
延伸閲讀
[編輯]- Markowicz-Piasecka M, Huttunen KM, Mateusiak L, et al. Is Metformin a Perfect Drug? Updates in Pharmacokinetics and Pharmacodynamics. Curr. Pharm. Des. 2017, 23 (17): 2532–2550. PMID 27908266. doi:10.2174/1381612822666161201152941.
- McCreight LJ, Bailey CJ, Pearson ER. Metformin and the gastrointestinal tract. Diabetologia. March 2016, 59 (3): 426–35. PMC 4742508
 . PMID 26780750. doi:10.1007/s00125-015-3844-9.
. PMID 26780750. doi:10.1007/s00125-015-3844-9. - Moin T, Schmittdiel JA, Flory JH, et al. Review of Metformin Use for Type 2 Diabetes Prevention. Am J Prev Med. October 2018, 55 (4): 565–574. PMC 6613947
 . PMID 30126667. doi:10.1016/j.amepre.2018.04.038.
. PMID 30126667. doi:10.1016/j.amepre.2018.04.038. - Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. September 2017, 60 (9): 1577–1585. PMC 5552828
 . PMID 28776086. doi:10.1007/s00125-017-4342-z.
. PMID 28776086. doi:10.1007/s00125-017-4342-z. - Sanchez-Rangel E, Inzucchi SE. Metformin: clinical use in type 2 diabetes. Diabetologia. September 2017, 60 (9): 1586–1593. PMID 28770321. doi:10.1007/s00125-017-4336-x.
- Zhou J, Massey S, Story D, et al. Metformin: An Old Drug with New Applications. Int J Mol Sci. September 2018, 19 (10). PMC 6213209
 . PMID 30241400. doi:10.3390/ijms19102863.
. PMID 30241400. doi:10.3390/ijms19102863. - Zhou T, Xu X, Du M, et al. A preclinical overview of metformin for the treatment of type 2 diabetes. Biomed. Pharmacother. October 2018, 106: 1227–1235. PMID 30119191. doi:10.1016/j.biopha.2018.07.085.
